As healthcare becomes increasingly digitalized, much of the care that is delivered in hospitals today will move into the home and the community. At the same time, hospitals will continue to play a pivotal role in the distributed healthcare system of the future, using smart technologies to provide the highest level of acute and specialist care to the most ill and complex patients. By coupling the power of data, AI, and IoT with human-centered design, hospitals can improve operational efficiencies, deliver clinical excellence, and create seamless patient experiences within and beyond hospital walls.
No patient wants to end up in hospital. But when they do, they want their experience to be as frictionless, comfortable, and reassuring as possible, with minimal waits and delays. Physicians and hospital staff, for their part, want to focus on delivering the best possible patient care, without getting bogged down in administrative duties or having to manually scramble together patient data.
The reality is that, despite impressive advances in medical innovation, hospital care today is all too often plagued by disconnects and inefficiencies that get in the way of optimal experiences and outcomes.
Information overload is a major issue, with 55% of healthcare leaders in the 2022 Philips Future Health Index report expressing concerns that their staff is overwhelmed by the volume of data available to them [1]. That data is often locked away in silos, hindering the ability to use it effectively. Burnout among healthcare professionals continues to be on the rise, with excessive administrative work being the main culprit [2]. Hospital leaders are facing growing shortages of qualified staff coupled with rising burnout rates – prompting them to consider how they can improve staff retention and satisfaction [3].
Inefficiencies exact a financial cost, too, in times when hospitals are operating on razor-thin margins. In the US, for example, it is estimated that 25% of healthcare spending is wasted through issues such as delayed discharge, poor transitions of care, and suboptimal asset management [4].
Meanwhile, patients are looking for easier ways to schedule hospital appointments and access their health data generated across care settings. In fact, 95% of patients aged 18-34 say they will switch providers if the digital experience doesn’t meet their expectations [5].
Modernizing hospital care for the digital age
Faced with these challenges and demands, hospitals that embrace the full possibilities of digital transformation will be best positioned to deliver superior care experiences and outcomes, while driving out inefficiencies from their processes to help healthcare professionals operate at the top of their license and regain the joy in their work.
Governments worldwide also recognize the need for modernizing hospital care. For example, in Germany, the Hospital Future Act, which came into force in 2020, has made 4.3 billion euros of funding available for new digital hospital infrastructures and initiatives. Countries like China, Japan, and Singapore are also betting big on IoT technologies, AI, and robotics to improve the quality of hospital care and ease staff shortages.
So what exactly makes a hospital smart and fit for the future?
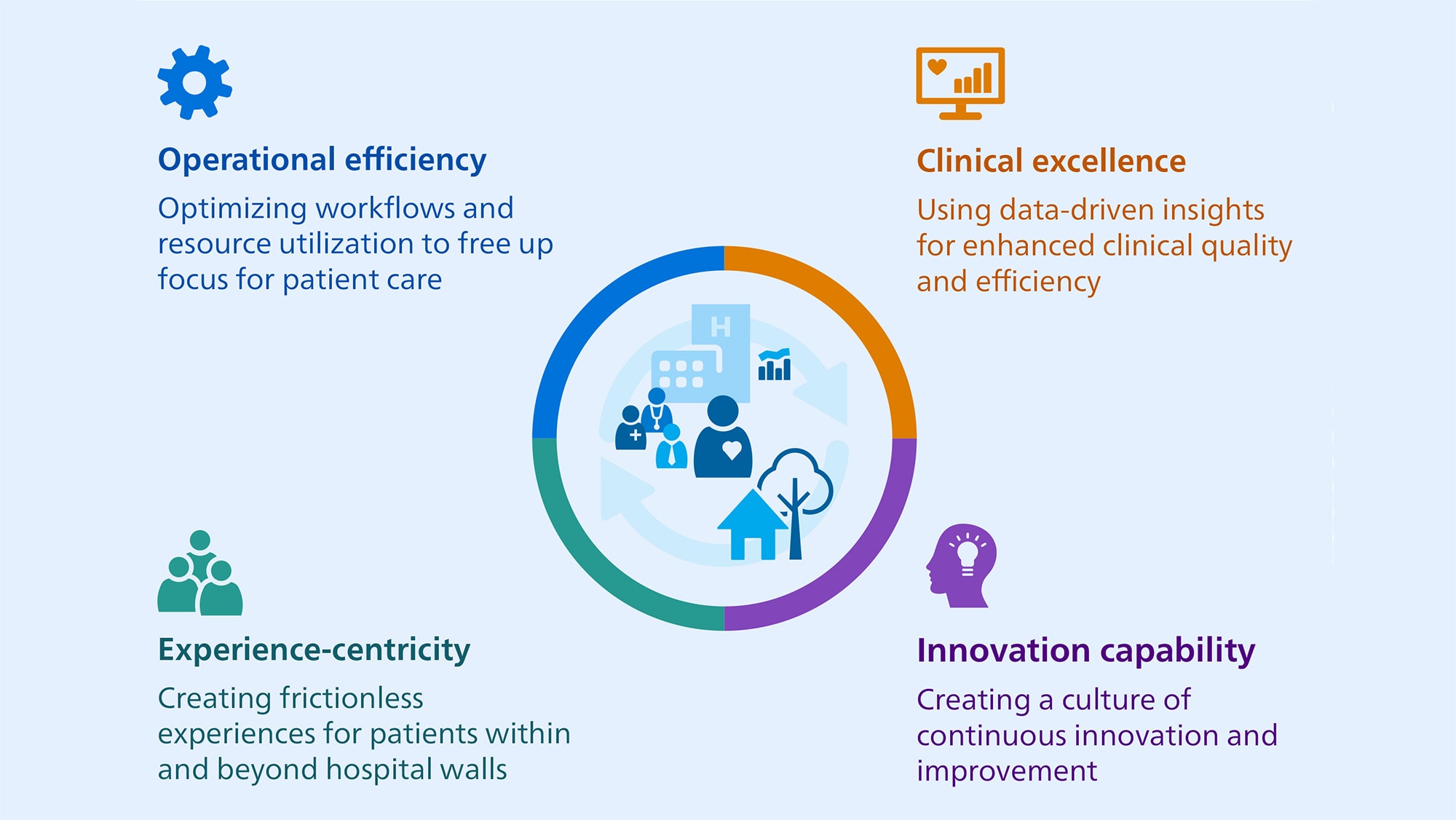
A smart hospital, as we envision it, connects people, data, and technology in intelligent ways to (1) improve operational efficiencies, (2) advance clinical excellence, and (3) create seamless patient experiences before, during, and after hospital visits – all of which need to be supported by (4) new capabilities to create a culture of continuous innovation and improvement.
In this post, we will focus on the first three aspects because the fourth warrants its own article.
Smart hospitals use automation to free up focus for patient care
One of the biggest opportunities afforded by smart technologies such as AI is to automate much of the cumbersome manual work that is wearing down physicians and staff. By adding intelligence to medical systems and devices, they also become easier to use for less-qualified staff, making hospitals less dependent on scarce specialists without compromising on quality and patient safety.
For example, in MR imaging, smart and touchless patient sensing technology can automatically check whether the patient position is correct and monitor a patient’s breathing – allowing the setup of routine MR exams to occur in less than a minute, even for less experienced operators, while helping them keep a caring eye on the patient. In addition, smart AI-enabled systems can suggest the most appropriate protocol for each MR exam, speed up image acquisition, as well as automate exam planning, scanning, and processing.
The point of such innovations is not to remove clinical and technical staff from the loop. It’s to equip them with actionable intelligence at their fingertips, with solutions that are deeply embedded into their workflows and designed to augment their capabilities. That means less time figuring out equipment settings, and more time interacting with the patient.

Another frequent source of frustration and inefficiency that automation can help to address is lack of real-time insight into asset location and utilization. For example, more than a third of nurses waste up to two hours a shift searching for missing medical equipment such as mobile infusion pumps [6].
Track-and-trace-like solutions – using physical tags combined with technologies such as WiFi, Bluetooth Low Energy, Infrared, or Radio Frequency Identification – can help staff find the nearest equipment more quickly and provide insights into equipment utilization. Using such a real-time location system, one Dutch hospital managed to identify the potential to save 20% on asset search times and 1 million euros on equipment investments based on more accurate utilization rates [7].
As a next step, real-time location data can be further enhanced with other information on equipment status and utilization, which smart and connected devices can transfer directly via WiFi. For example, when a device needs repair or maintenance, an automatic work order can be triggered in the hospital’s maintenance management system based on changes in device status and/or location, thereby enabling a more streamlined workflow and reduced downtime.
Real-time location tracking can also be used to follow patients throughout their care journey, for example as they move through the emergency department (ED). This can help answer question like: How much time do patients spend in the triage room? How long do they have to wait for their radiology exam? Early pilots have shown how such real-time information, integrated with data from other hospital systems such as the EMR, can help administrators manage patient flow in the ED as well as optimize equipment and bed utilization [8].
Over time, these track-and-trace-like solutions will evolve into enterprise-wide IoT platforms, allowing central command centers to manage transitions of care from one setting to the next based on accurate and real-time information about patients, beds, and equipment. Coupled with predictive analytics, this can help hospitals forecast and prevent bottlenecks in patient flow before they occur, thereby reducing waits and delays across the hospital and ensuring timely discharge for home-based monitoring.
Ultimately, we envision the smart hospital as a fully interconnected and intelligent system that can dynamically adapt in the moment, making staff and equipment available where they are needed most – for example when a disaster or local incident occurs. With the logistical challenges of the COVID-19 pandemic fresh in mind, this will help hospitals become more resilient in the face of future crises.
Smart hospitals integrate patient data to drive clinical excellence
Just like smart technologies can bring more insight, predictability, and efficiency to hospital operations, they can also help clinicians deal with a growing deluge of often disconnected patient data to support more integrated and efficient precision diagnosis and care.
Take cancer care, for example. As we advance our understanding of cancer, more and more patient information is becoming available to clinicians – including various medical images, pathology reports, genomics, and molecular test results. Pulling all that information together manually can be time-consuming and is also prone to error.
In collaboration with our clinical innovation partners, including Karolinska University Hospital in Sweden, we have developed digital dashboards that automatically integrate patient information from different sources for collaborative decision-making. As a result, we have been able to improve the efficiency of multidisciplinary tumor board meetings at Karolinska University Hospital through a 24% reduction in time spent per patient case, without compromising on patient outcomes [9].

Similarly, in acute and post-acute care, we are investing heavily in patient care management solutions that can integrate data from a plethora of monitoring devices and then filter that data intelligently for clinical use. With an ever-growing list of tasks constantly competing for attention, nurses and physicians don’t have time to go through large amounts of disparate data. They need timely and contextually relevant insights that they can act on in the critical moments that matter. For example, by pioneering the use of automated early warning scores that pick up on signs of patient deterioration in the general ward, one hospital was able to reduce the number of serious adverse events in patients by 35% [10].
In the smart hospital of the future, we will see more and more wireless patches – or even contactless, light-based sensing – enabling ubiquitous patient monitoring throughout the hospital. Mobile connected devices will reduce dependency on bedside equipment, making care teams more flexible to move around as needed. Avatar-based monitoring can further reduce cognitive load by integrating patient data in a highly visual way, providing an at-a-glance overview of their health status. All of this will be supplemented by remote guidance and mentoring from highly trained specialists in centralized hubs; a model that has already proven its value through tele-ICUs, and which could also support staff in lower-acuity areas such as the general ward.

Smart hospitals design for seamless end-to-end patient experiences
With smart technologies offering so many possibilities to optimize hospital care, it’s the ability to create seamless patient experiences across their care journey that ultimately glues everything together. And in the smart health system of the future, that journey starts well before the patient enters the hospital.
Digital self-triaging can help patients assess their symptoms and determine the next best step. Online self-scheduling allows them to book an appointment just as easily as they would book a taxi or a flight. And by sharing educational content with patients in advance, going into the hospital no longer needs to be a step into the unknown. Patients will know what to expect and feel more at ease as a result. Personalized reminders can help ensure they arrive in time, reducing no-shows by up to 42% [11].
Once patients arrive at the hospital, a virtual waiting room allows them to check in using their mobile phone and get notified when the doctor is ready to see them. Digital wayfinding can guide patients through the hospital, helping them get to their appointment without stress.
For patients who need to undergo an exam or procedure, ambient experience solutions can provide further information and guidance during scanning or prior to the procedure, while offering a personalized audiovisual experience that puts patients at ease – including young children. In MR imaging, this has been shown to reduce re-scans by as much as 70%, improving clinical efficiency as well as patient experience [12].

In the future, combining ambient experience with smart contactless sensing will allow hospitals to create increasingly adaptive healing rooms and environments, for example by adjusting the lighting or temperature based on patient’s stress levels. As a result, hospital rooms will offer patients a greater sense of comfort and well-being, promoting speedy recovery and patient satisfaction.
At the same time, as we outlined in our previous post, remote patient monitoring will allow patients to resume living the lives they love more quickly, without occupying a scarce and expensive hospital bed any longer than needed. Clinical oversight from virtual care teams will help spot early signs of health deterioration to enable timely and targeted intervention.
The smart hospital of the future will not be bound by walls – it will offer seamless experiences that follow the patient wherever they go, all while improving clinical and operational efficiencies to help healthcare professionals focus on what drew them to medicine in the first place: delivering better care to patients.
Download our position paper on digital transformation in healthcare
Discover what the future of digital health will look like – and what is needed to turn this vision into a reality.
References
[1] Philips Future Health Index 2022 report: https://www.philips.com/a-w/about/news/future-health-index/reports/2022/healthcare-hits-reset
[2] https://www.prnewswire.com/news-releases/medscape-physician-burnout--depression-report-2022-shows-pandemics-continued-impact-301465333.html
[3] Philips Future Health Index 2022 report: https://www.philips.com/a-w/about/news/future-health-index/reports/2022/healthcare-hits-reset
[4] Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA.2019;322(15):1501–1509. https://jamanetwork.com/journals/jama/fullarticle/2752664
[5] https://econsultancy.com/consumers-expect-digital-services-healthcare-providers/
[6] https://www.nursingtimes.net/archive/nurses-waste-an-hour-a-shift-finding-equipment-10-02-2009/
[7] https://www.philips.nl/a-w/about/news/archive/standard/about/news/press/2020/20201027-philips-introduceert-performanceflow-een-nieuwe-digitale-oplossing-voor-slim-beheer-gebruik-en-aanschaf-van-mobiele-medische-apparatuur.html (in Dutch)
[8] https://www.philips.com/c-dam/b2bhc/de/consulting/performanceflow/2021-11_Philips_PerformanceFlow_Whitepaper_Smart_Asset_Management.pdf
[9] https://pubmed.ncbi.nlm.nih.gov/35922094/
[10] https://www.philips.com/a-w/about/news/archive/case-studies/20180315-early-warning-score-reduces-incidence-of-serious-events-in-general-ward.html
[11] https://europepmc.org/article/med/31298628
[12] https://www.philips.com/a-w/about/news/archive/standard/news/articles/2020/20201201-philips-ambient-experience-better-imaging-precise-diagnoses-and-better-patient-care.html
Share on social media
Topics
Author

Henk van Houten
Former Chief Technology Officer at Royal Philips from 2016 to 2022

Sean Carney
Former Chief Experience Design Officer at Royal Philips from 2011 to 2022












