Jul 30, 2024
Philips Future Health Index 2024 Australia Report: Technology, AI and partnerships bridging gaps toward a more equitable and sustainable healthcare system
Sydney, Australia – Royal Philips (NYSE: PHG, AEX: PHIA), a global leader in health technology, today released the Australia findings of its Future Health Index (FHI) 2024 report : Better care for more people. The ninth edition of the report, which surveyed nearly 3,000 healthcare leaders in 14 countries, including Australia, shows that Australian healthcare leaders are addressing ongoing workforce shortages, increasing financial burdens and urgent demand to deliver high-quality care. By focusing on innovative solutions in virtual care, automation and data analytics empowered by AI, they are taking steps to overcome these challenges whilst working with industry partners and government towards a more equitable and environmentally sustainable healthcare system.
In response to the report findings, Matt Moran, Managing Director, Philips Australia and New Zealand, said: “Whilst timely access to high-quality care remains under pressure, healthcare leaders are leveraging technology and collaboration to overcome these hurdles. Their efforts are demonstrating that next-generation data integration, virtual care and strategic partnerships can significantly improve the quality and accessibility of healthcare for all Australians. At Philips, we are committed to supporting these initiatives by providing innovative solutions that enhance patient care, streamline workflows and foster sustainable practices. Together with our partners, we are working towards a healthcare system that is not only efficient but also resilient and equitable.”
Automation, virtual care and remote patient monitoring help alleviate staff shortages
More than three quarters (78%) of healthcare leaders in Australia report delays in care are an issue at their organisation due to staff shortages. Pressure from these shortages has resulted in deteriorating staff well-being, declining mental health and work-life balance (47%), higher patient-to-staff ratios (32%), insufficient time with each patient (28%) and increased clinical errors (27%). 97% of leaders say their organisations are facing financial challenges that hinder their ability to provide timely, high-quality care, further exacerbating the impact of staff shortages.

In response to these challenges, automation is emerging as a solution for improving staff availability and well-being. Almost all (98%) healthcare leaders in Australia believe automation is critical for addressing staff shortages by automating repetitive tasks or processes, among the highest result from all 14 countries surveyed. The same number (98%) agree automation will save healthcare professionals time by reducing their day-to-day administrative tasks.
Virtual care also plays a role in managing staff shortages. Almost all (98%) leaders report integrating virtual care has helped ease staff shortages at their organisations. Three in four (75%) have seen virtual care directly support healthcare professionals, whether by increasing staff support for complex patient management (39%), expanding specialist care to underserved communities (33%) or improving collaboration between healthcare professionals in different locations (32%).
Healthcare leaders in Australia turn to virtual care to reach remote communities. They are more likely than the global average, APAC average and US participants to already use remote patient monitoring for elderly care (60%), maternal and foetal care (55%) and post-operative monitoring (55%).
Whilst timely access to high-quality care remains under pressure, healthcare leaders are leveraging technology and collaboration to overcome these hurdles. Their efforts are demonstrating that next-generation data integration, virtual care and strategic partnerships can significantly improve the quality and accessibility of healthcare for all Australians.
Matt Moran
Managing Director, Philips Australia and New Zealand
One example of this approach is the Health in a Virtual Environment (HIVE) program in rural Western Australia. Overseen by the East Metropolitan Health Service (EMHS) and developed by Philips, HIVE uses early detection AI technology and remote monitoring to improve care for high-risk, acute inpatients.
HIVE provided continuous remote monitoring over 2.5 years for 7,500 high-risk inpatients, accumulating 300,000 hours of monitoring, according to a recent study by the University of Western Australia and EMHS. This virtual care has reduced hospital stays, cut waiting times for beds, freed up staff time and lowered costs. In a 12-month period, there were more than 10,000 interactions between the HIVE team and bedside staff, demonstrating the program’s effectiveness in supporting healthcare professionals in rural areas.
It thus comes as no surprise that almost all (90%) of Australian healthcare leaders believe patients at their organisation are positive towards virtual care, ahead of the global average of 72%. They plan to expand applications of remote patient monitoring in many areas at a higher rate than their peers overseas: 38% currently use remote patient monitoring for telestroke care and an additional 50% plan to implement it for this application in the next three years, as example.
AI-enabled clinical decision support in healthcare faces data integration hurdles
Survey participants recognise that using data-driven insights can help improve service to their communities. Leaders identify opportunities for these insights in optimising treatment plans and care pathways (41%), forecasting and managing patient demand (36%) and identifying evidence-based best practices (35%). Data-driven insights are also seen as instrumental in supporting evidence-based policy decisions (38%), helping reduce disparities in health outcomes between communities.
However, nearly all leaders (97%) report facing at least 1 data integration challenge that impacts their ability to provide timely, high-quality care. These challenges include an increased risk of errors (34%) and missed opportunities for preventive care or early intervention (32%). Increased operational costs due to inefficiencies concern 32% of leaders, whilst 26% report that the time spent accessing and integrating data results in less time available for patient care.
Healthcare leaders suggest that if their organisations are to make the most of the latest innovations, including AI, they need to see changes such as improved accuracy of patient data (35%) and improved interoperability between different platforms and healthcare settings (32%).
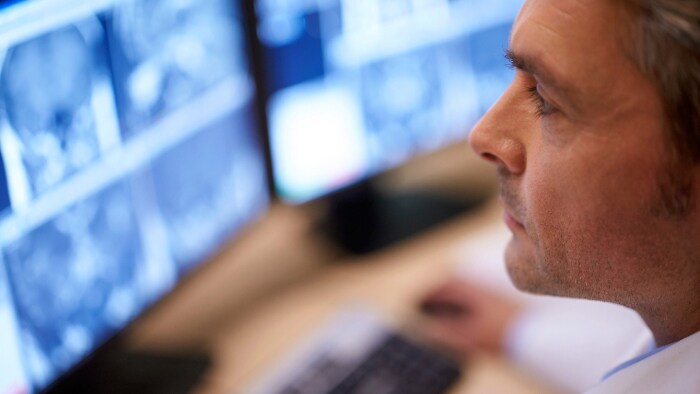
Australian healthcare leaders are more likely than the global average to have already implemented AI for clinical decision support in 7 out of the 8 areas listed in the survey. Top among these are AI for clinical decision support in in-hospital patient monitoring (59%), preventive care (58%) and treatment planning (55%). These trends look set to accelerate with 43% of healthcare leaders planning to implement AI in clinical command centres; 41% for radiology and medication management; 40% for remote patient monitoring; and 34% for in-hospital patient monitoring in the next three years.
Additionally, healthcare leaders seemingly recognise that generative AI reflects innovation that could help unlock new efficiencies and insights from patient data. Nearly half (47%) of leaders surveyed are currently investing in generative AI technologies, and 39% more plan to invest by 2025.
Despite these advancements, nearly all leaders (95%), express concern about the possibility of data bias in AI applications widening disparities in health outcomes. To mitigate this risk, they are calling for greater transparency and interpretability (46%) supported by continuous staff training and AI education (39%) and ensuring staff diversity in data and AI (40%).
Our role is not just about the health of people, but also the health of the planet.
Angie Bone
Associate Professor, Monash Sustainable Development Institute
Collaboration and partnerships key to environmentally sustainable and quality healthcare
Confronted with myriad systemic challenges, more than one in three healthcare leaders (36%) believe partnerships are essential for delivering better care to more patients whilst also caring for the planet. Forty-seven percent see a vital role for health technology companies in improving the timeliness and quality of care delivery. Key areas where external partnerships are needed include improving care coordination (36%), attracting and retaining staff (34%), enhancing technology integration and interoperability (33%) and using data analytics for informed decision-making (30%).
Collaboration is also recognized as crucial to accelerate progress towards a climate-resilient, carbon-neutral healthcare sector. 99% believe that reducing CO2 emissions and the environmental impact of healthcare should be a top priority for healthcare organisations and the government.
Reflecting this sentiment, Angie Bone, Associate Professor at Monash Sustainable Development Institute, emphasised the broader responsibility of healthcare leaders during the CEDA healthcare sustainability panel: “Our role is not just about the health of people, but also the health of the planet.”
Leaders acknowledge that addressing the sector’s environmental impact is no longer a matter of if, but how. Many have already implemented sustainability strategies related to energy (78%), supply chain (76%), equipment (74%), and emission reductions (70%).
By reducing their carbon footprint, healthcare organisations can achieve savings that benefit both the environment and their bottom line. Almost all Australian healthcare leaders (97%) report that environmental criteria play a role in their sourcing or tendering processes, although only 17% always have green criteria in procurement. Additionally, 84% have set targets for decarbonisation and tracking emissions or plan to do so within the next three years. However, nearly one in five (17%) either do not have plans for decarbonisation or are unsure about their plans.
Highlighting the importance of these collaborations, Kylie Woolcock, CEO of the Australian Healthcare and Hospitals Association, stated during a virtual panel of international healthcare leaders for the Committee for Economic Development of Australia (CEDA): “Partnerships are critical in this space. It’s one thing to have a shared vision or outcome, but managing the imbalance in information and expertise across both sustainability and technology spaces is crucial.”
Partnerships are critical in this space. It’s one thing to have a shared vision or outcome, but managing the imbalance in information and expertise across both sustainability and technology spaces is crucial.
Kylie Woolcock
CEO, Australian Healthcare and Hospitals Association
About Royal Philips
Royal Philips (NYSE: PHG, AEX: PHIA) is a leading health technology company focused on improving people's health and well-being through meaningful innovation. Philips’ patient- and people-centric innovation leverages advanced technology and deep clinical and consumer insights to deliver personal health solutions for consumers and professional health solutions for healthcare providers and their patients in the hospital and the home. Headquartered in the Netherlands, the company is a leader in diagnostic imaging, ultrasound, image-guided therapy, monitoring and enterprise informatics, as well as in personal health. Philips generated 2022 sales of EUR 17.8 billion and employs approximately 77,000 employees with sales and services in more than 100 countries. News about Philips can be found at www.philips.com/newscenter.











