One in 10 people undergo a surgical procedure each year [1]. That means that over the next decade it’s highly likely you – or someone close to you – will too. This may sound like a scary prospect, but it doesn’t have to be.
That’s because we’re making huge strides forward in innovation that I believe will make your operation more likely to be a medical success while having a better experience along the way.
Got five minutes? Because I’d like to show what I think the future of surgery will look like in a decade.
Getting you back to living the life you love faster, safer, and with less anxiety
If you need to see a doctor in 2033 for a major disease, you could be diagnosed and treated in one single room on the same day. This could include medical emergencies like a heart attack or a stroke or long-term diseases like lung cancer or disorders of the spine, for which many patients today have to wait weeks, or even months, for treatment.
In 10 years’ time, your care could be radically improved thanks to advances made by combining cutting-edge technologies into one intelligent room. This is a room that gives doctors like me almost superhuman abilities, enabling us to treat some of the most common and most life-threatening diseases in one go. I’m talking about an entire room that will be powered by a mix of photo-realistic Augmented Reality (AR), robotic automation, artificial intelligence (AI), ultra-high resolution 3D medical imaging and smart devices that all talk to one another. It will enable doctors to perform operations with less damage to your body, less time spent in the hospital, a faster treatment and recovery, and in some cases, immediate diagnosis and treatment.
Today, we can already do some of these procedures thanks to a combination of technologies called Image-Guided Therapy, or IGT for short [2]. IGT is essentially modern-day surgery that uses minimally invasive techniques to allow me to do what surgery used to do (by cutting you open, which is far more dangerous and requires more time to recover). IGT procedures are carried out through incisions not much larger than a pencil point, leaving behind just a band aid.
Imagine that it’s 2033. Let’s look at four of the world’s most common diseases in four different countries and explore how your care will be radically different:
1. Care will be faster
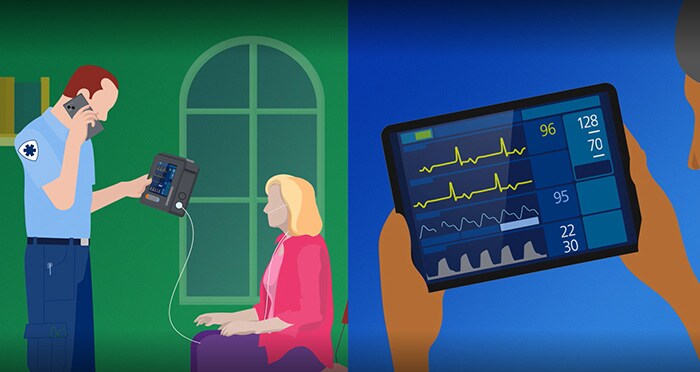
The paramedics are at your home somewhere on the U.S. East Coast. They suspect a stroke, but it could also be a number of other things. Fortunately, their hand-held monitor can now connect them to the hospital and instantly to a stroke expert who reviews your monitoring data and confirms that you’re having an acute cerebral event, possibly an ischemic stroke.
The paramedics rush you to the hospital, where CT scans are taken and then reviewed by a remote neurologist, who quickly confirms your diagnosis and sends you to treatment.
So far, only 45 minutes have passed since your stroke began. Every minute that a stroke goes untreated results in the death of 2 million neurons. Every 30 minutes’ delay before treatment reduces the chance of a good outcome by 14%. And each hour of delay ages your brain by 3.6 years [5]. Time is literally brain [4].
Luckily, you get to us within the golden window – the earliest hours following a stroke when we can reduce or even reverse the long-term effects. Scans confirm the diagnosis, so I make a pencil-point incision in your thigh. I touch a hologram of an artery in your neck and in seconds the device (with the aid of robotics) rapidly threads itself along your arteries to a tiny clot that is cutting off blood flow to your brain. Within just minutes, we have removed the clot.
Through my AR glasses, I can clearly see that the blood flow has been restored, reversing the stroke-in-progress and preventing any devastating long-term effects. All while an expert from Tokyo was watching your entire procedure through her AR glasses and sharing her clinical advice. You are then whisked to recovery bays in the neuro intensive care unit. You’ll be home having dinner with your family within 48 hours.
2. Care will be “one and done”
Perhaps you live in the Netherlands, and you’re in the operating room with my colleague Jess because you’ve been referred for a suspicious spot towards the base of your left lung. Less than one hour later, Jess has diagnosed and destroyed all of a tiny tumor in one go without opening up your body.
How? It turns out you had lung cancer, a disease that kills more people than breast cancer, prostate cancer and colon cancer – combined. In the Netherlands alone it kills more than 10,000 people every year [6].
In 2033, Jess is able to look at your lungs on her AR screen and see every detail within and around your lungs in sharp focus. She pinpoints precisely where the cancerous cells are that need destroying. She virtually sculpts a 3D model of an AI-predicted kill zone around the tumor, and she then destroys the cells using microwave energy.
When you wake up, instead of facing a six-month waiting period before follow-up scans to see if it is an early cancer that is growing, you find out immediately its all-clear.
One and done. How amazing is that?
3. Care is closer to you
We have a saying in the medical world: Save a limb, save a life. This is something we’re doing much more easily in 2033. Even if you live far away from a city.
Take Australia for example, where almost a third of the population still lives in rural areas. Even though the country has more hospital beds per capita than the U.S. or the U.K., hospitals are desperately overcrowded, and patients face a huge increase in waiting time for elective surgeries.
So instead, we come to you. In the U.S., physicians like me have been using office-based labs, or OBLs, for decades to perform routine procedures like the removal of fibroids, or even minimally invasive operations on your heart. And they’re fantastic because they enable doctors to take care outside of hospitals and bring it closer to the communities and patients that we serve.
In 2033, we put our highly-intelligent IGT rooms into mobile OBLs – creating what’s essentially a hospital on wheels, with doctors inside who can carry out elective procedures on your doorstep. Procedures to treat things like peripheral artery disease (PAD), or poor blood circulation in the leg, which causes cramping and pain when you walk. Incredibly, nearly a quarter of a billion people suffer from PAD worldwide [7]. If left untreated, it can lead to amputation, which in turn raises your risk of dying. But with mobile OBLs, we’re making sure to reach our patients who find it hard to get to us.

A hospital on wheels from mobile medical program Heart of Australia
4. Care is safer for you (and me)
If you live in India, you almost certainly know someone with cardiovascular disease (CVD). That’s because CVDs are more common, especially among the younger population [8]. Replacing an aortic valve in your heart used to require massive surgery, splitting the chest open, lots of blood loss, lots of days in the hospital. In 2033, we can do this through a minimally invasive procedure called transcatheter aortic valve replacement (TAVR).
And in 2033, our intelligent surgical rooms will include a groundbreaking technology that uses light rather than X-rays to let me navigate through the body in real-time and in 3D, from any angle. So not only can I perform a TAVR through a tiny incision in your groin, but you go home the same day and there’s no radiation, making it safer for both you and me.

A minimally-invasive aortic heart valve replacement (TAVR)
More accessible care for everyone
I started this story by saying that one in 10 of us will need surgery over the next decade. Now let’s end on a positive note: at Philips, our minimally-invasive solutions already help doctors worldwide to treat one patient every second of every day. Which means since you started reading this blogpost, more than 400 people have had their tumors killed, their strokes reversed, and their hearts and blood vessels mended using our technology. And because every single innovation you’ve just read about is being developed right now, I’m confident we’re well on the way to getting even more of you – and the people you care about – back to living the lives you love.
As futures go, that’s literally life-changing.
To learn more about developments in minimally invasive procedures and the future of health, follow me on LinkedIn @AtulGupta_MD
Sources:
[1] https://academic.oup.com/bja/article/119/2/249/4049141
[2] https://www.youtube.com/watch?v=BAt-akrOw_o&list=PL3WBa0emAbeJCS4_zCZ4KuHz9JH-_ChTV&index=2
[3] Emory University
[4] [PDF] Time Is Brain—Quantified | Semantic Scholar
[5] ncbi.nlm.nih.gov/pubmed/16339467
[6] https://www.jto.org/article/S1556-0864(20)30821-2/fulltext
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6113064/#:~:text=It%20is%20estimated%20that%20%3E200,symptoms%20from%20none%20to%20severe.
[8] https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds),
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994761/
Share on social media
Topics
Author

Atul Gupta
Chief Medical Officer, Image Guided Therapy Atul Gupta, MD is Chief Medical Officer at Philips’ Image Guided Therapy and a practicing interventional radiologist. Prior to joining Philips in 2016, Atul served on Philips’ International Medical Advisory Board for more than 10 years. Atul continues to perform both interventional and diagnostic radiology in suburban Philadelphia, in both hospital and office-based lab settings. He has been repeatedly recognized as top physician for his specialty in the media and serves on several advisory boards. He has also published and lectured internationally on a range of interventional procedures.
Follow me on




