Jun 08, 2017
Future Health Index, a global study by Philips, finds misconceptions about the cost of connected care inhibit its uptake
Sydney, Australia – Commissioned by Royal Philips (NYSE: PHG, AEX: PHIA), the Future Health Index, which surveyed more than 33,000 individuals across 19 countries, has found Australia is behind when it comes to integration across the healthcare system and adoption of connected care technologies, compared to the 19-country average. A large portion of both the general population and healthcare professionals (HCPs) polled in Australia perceive potential long term cost increases associated with both integration and adoption, which could act as a key barrier to implementation and use. Across Australia the study surveyed around 1,500 general population and 200 HCPs. According to the research, both groups recognise the importance of integration and connected technologies in improving healthcare in Australia. 87% of HCPs and 76% of the general population believe it is important that the healthcare system in Australia is integrated. In addition, 73% of HCPs and 74% of the general population agree connected care technology is important for preventing medical issues. Kevin Barrow, Managing Director, Philips Australia and New Zealand said the 2017 Future Health Index highlights that both industry and the public are receptive to increased integration and further adoption of connected care devices. “In order to create and maintain a sustainable healthcare system, industry and policy in Australia need to shift towards wrapping care around the patient with greater emphasis on prevention and patient ownership. We need to move away from the current episodic diagnosis and treatment model. The way to achieve this is to seek out efficiencies through improved integration and adoption of connected care technologies, to empower people to take more preventive measures and to proactively manage their health,” he said.
Performance across the indices The Index evaluates the readiness of countries to address pressing health challenges by measuring the perceptions and experiences of the key users of healthcare systems across the access to healthcare, integration of the health system, and adoption of connected care technologies. Efficiency in Australian healthcare The study also produced an efficiency ratio to compare healthcare expenditure as a percentage of GDP with health outcomes, providing a snapshot of how healthcare spending is ultimately impacting the health of the population. Australia’s efficiency ratio falls below the 19-country average of 10.5 at 9.5, indicating the outcomes achieved by the healthcare spend are not optimal. “Australia’s current approach to healthcare has afforded the population great access and results, but it has come at high cost. Healthcare spend in Australia as a percentage of GDP is 9.4, compared to the global average of 8.7. If this above average spend was matched with efficiency equally above average, we’d be in a much better position, but it’s not. The reality is that we still need better integration and the adoption of healthcare technologies to facilitate a more efficient value-based model of care,” said Barrow. Australia’s performance across the indices and in terms of efficiency highlights the potential for improved integration and adoption of connected care technologies to increase Australian healthcare efficiencies. “There are pockets of innovation in Australia, where the current delivery of care is being disrupted by connected technologies and we are starting to see value-based models introduced. We need to use these examples to illustrate the benefits of such technologies and apply these models more broadly,” said Barrow. Philips’ partnership with West Moreton Hospital and Health Services (WMHHS) is one such example of leading local innovation. The recently introduced Mobile Enabled Care (MeCare) has delivered a user-friendly, connected health management program that provides in-home continuous monitoring and care for people with chronic health conditions. The program recently has won a Queensland Health eAward in the Clinical Innovator category. Dr. Kerrie Freeman, WMHHS Interim Chief Executive, said there is a significant role for technology in enabling the future delivery of care. “With the growing number of studies into effectiveness of healthcare delivery models for patients, adapting new innovations in the care setting is important. As the pressures on the health system continue to grow, we will need to continue to deliver better quality care by harnessing technology opportunities to improve the cost, quality and outcomes of care for the community. That is one of the key drivers for the MeCare program. It offers a new model of care, through which we are able to connect patients with services remotely and improve quality of life, prevent Emergency Department presentation and inpatient admission, ultimately easing burden on the system,” Dr. Freeman said. To download the 2017 Future Health Index report in its entirety, please visit here. For additional Future Health Index related content, please visit here. For the Australian summary of the report commissioned by Philips, please visit here.
About Royal Philips
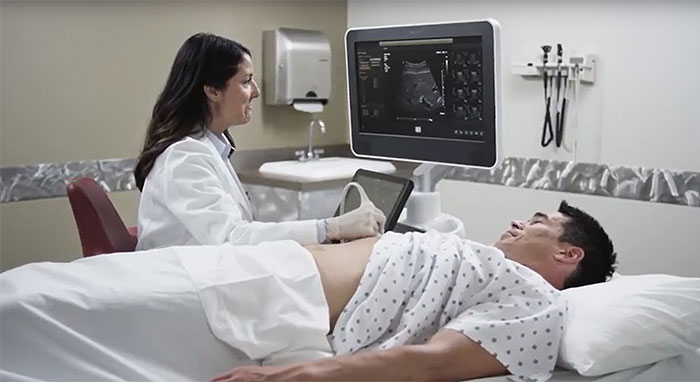
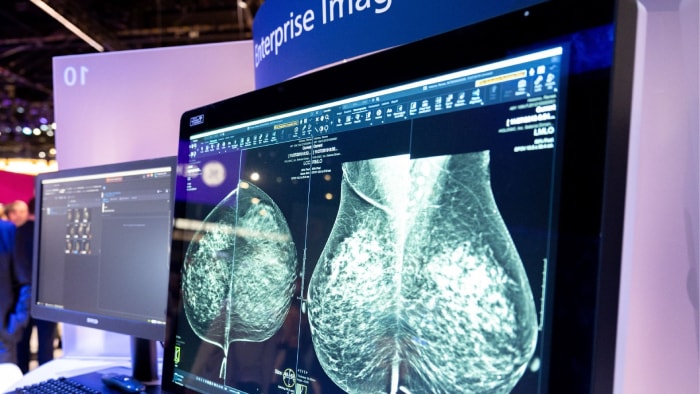
Royal Philips (NYSE: PHG, AEX: PHIA) is a leading health technology company focused on improving people’s health and enabling better outcomes across the health continuum from healthy living and prevention, to diagnosis, treatment and home care. Philips leverages advanced technology and deep clinical and consumer insights to deliver integrated solutions. Headquartered in the Netherlands, the company is a leader in diagnostic imaging, image-guided therapy, patient monitoring and health informatics, as well as in consumer health and home care. Philips’ health technology portfolio generated 2016 sales of EUR 17.4 billion and employs approximately 71,000 employees with sales and services in more than 100 countries. News about Philips can be found at www.philips.com/newscenter.
Topics
Contacts

Albertine Schor Brand and Communications Manager Tel: +61 (02) 9947 0040