Five reasons why healthcare providers are adopting as-a-service models in patient monitoring
Jun 20, 2023 - Reading time 7-9 minutes
Healthcare leaders often struggle to keep up with constant changes in technology. Meanwhile, staff are burdened with disconnected systems and workflows that pull their attention away from the patient. As-a-service models are emerging as a new and cost-effective way of addressing these and other challenges, giving healthcare providers up-to-date capabilities while improving the staff and patient experience through better integration of data and technology.

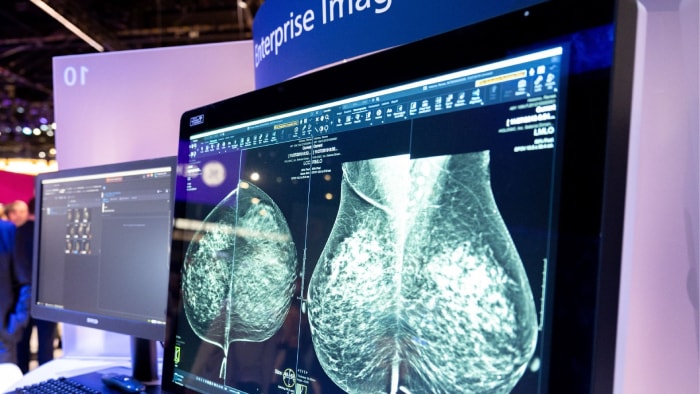
We have seen the same trend play out in many industries, from transportation to software and entertainment. People and companies used to buy and own products. Now, they can access the latest offerings through flexible, subscription-based consumption models, which often come with full-service packages and regular updates that offer additional value over time [1]. And this trend is showing no sign of slowing down. As digital transformation continues to accelerate across industries, we are rapidly moving to a world where Everything as a Service (XaaS) will be the new norm [2]. Nowhere is this need more evident than in patient monitoring. As the second most impactful IT investment in the delivery of care (behind electronic medical records, or EMRs), patient monitoring systems have always been a priority for healthcare leaders. However, the COVID-19 pandemic underscored the need for increased flexibility and scalability to meet dynamic shifts in patient demand. It also highlighted the many disconnects – between data, systems and workflows – that can get in the way of providing optimal patient care. In the past few years, patient monitoring has therefore evolved from being focused simply on ‘equipment management’ to more broadly ‘system optimization’ that supports standardization and integration of workflows across departments and facilities [3]. Monitoring as a service has been shown to be a powerful enabler of this transformation. Here are five reasons why a growing number of healthcare leaders are considering it as a new partnership model:
In healthcare too, care providers are shifting away from procuring medical equipment, software, and infrastructure separately. Instead, they are increasingly looking for integrated solutions that meet their needs at a departmental or enterprise level. What’s more, they want these solutions to be delivered as-a-service, giving them up-to-date capabilities that seamlessly work together to support their clinical, operational, and financial goals – without the traditional burden of equipment management.
1. Relieving the burden of technology management in patient monitoring
With traditional business models, hospitals purchase patient monitoring systems, after which they are responsible for the ongoing maintenance, security, upgrades, and user training across their networks. As patient monitoring technology keeps advancing, this creates a substantial burden for hospitals to keep up with the pace of innovation and remain compliant. Over time, the result is often a patchwork of disconnected systems – different monitors, from different vendors, and with different software revision levels – which require constant effort to keep everything performing to standards. Monitoring as a service takes much of this burden away. It can give healthcare providers access to the latest patient monitoring systems and healthcare informatics solutions, thereby helping to standardize patient monitoring at all acuity levels and across all care settings. It can also include ongoing software updates, system maintenance, and security patching – offering a flexible level of service and support that can be tailored to the hospital’s needs. Having standard interfaces and workflows also makes it much easier to train new and existing staff on the use of monitoring technology, further supporting continuity of operations. As a result, healthcare leaders can move beyond a reactive mode where technology is something they need to keep going, to a proactive mode where they can shape and control how technology is used to improve patient care.

2. Predictable volume-based costs
There is also a significant financial benefit to monitoring as a service. For many hospitals, rapid changes in technology are outpacing budget availability. Replacing or updating a patient monitoring system can consume substantial upfront capital resources. Compounding the issue is that healthcare leaders often lack utilization data on installed systems, making it difficult to understand what exactly they are paying for, what value it provides, or what staff are using (and in some cases, not using). Especially in the current challenging economic climate, it is no wonder that healthcare leaders are seeking alternatives to keep their systems up to date without straining their budgets. The Philips Future Health Index 2023 report showed that more than one-third (34%) of them are looking to mitigate financial pressures by exploring new purchasing models. With an as-a-service approach, healthcare leaders no longer need to consider how they might finance a significant upfront cost of a clinical system as a capital expenditure. Instead, they have a predictable fee to pay each month as an operating expense, tied to patient volume. Because an as-a-service model gives them more insight into how technology is used by staff and how it impacts the quality of patient care, they can also become more strategic about their investments.
3. Adaptability to meet fluctuating patient demand
If there is one thing that hospitals have learned from the COVID-19 pandemic, it is the need for increased flexibility to match unpredictable fluctuations in patient demand. As-a-service models allow healthcare providers to rapidly scale up or down their patient monitoring capabilities without large upfront capital expenditures. During the pandemic, this enabled hospitals to pivot quickly in reaction to changes in patient volumes and acuity levels, so they could meet the needs of both patients and staff. Thanks to the ability to see, at a glance, where monitors were and how they were being used, these monitors could be quickly relocated to COVID-19 units without impacting other patients’ care [4]. Coming out of the pandemic, this kind of adaptability will continue to serve hospitals well as they seek more flexible patient monitoring capacity. This will, for example, enable them to respond more quickly to a local traumatic event that causes a spike in patient demand. The increased flexibility that comes with as-a-service models also allows hospitals to scale solutions more easily across units, departments, and networks at large – making these solutions available when and where they are needed.

4. Improved data and workflow integration
For physicians and nurses, one of the biggest challenges in acute care today is the huge cognitive burden that comes from having to manage an overload of information from disparate systems. The need for manual data transfer adds to this burden. Patient monitors are often still disconnected from a hospital’s EMR system, keeping patient data locked in silos. Lack of consistent workflows can also lead to variable clinical quality. Through monitoring as a service, healthcare leaders can start building a more connected and integrated technology ecosystem with support from an enterprise technology partner. Improved interoperability allows data to be shared more easily between the EMR and other informatics systems, while standardization of equipment and workflows can help reduce variability in quality of clinical care. Monitoring technology fades into the background, helping staff to focus on providing patient care. The results can be significant. For example, one hospital reported 13,331 potential hours saved annually through automation and workflow improvements, as well as eight hours of daily time savings related to automated measurement and data exporting. Through these and other improvements, staff satisfaction with patient monitoring systems increased from 8% to 90% [5].
5. Continuous data-driven performance optimization
Next to supporting integration of clinical data at the point of care, a monitoring-as-a-service partnership can also offer healthcare leaders the insights they need for continuous data-driven improvement at a departmental or enterprise level. For example: how does the rate of equipment utilization or protocol adherence vary between units? And how does this inform where more staff training, or other interventions, may be needed? With traditional transactional models of procuring equipment, healthcare leaders often lack these kinds of insights, leaving them in the dark about potential improvements. By adopting an as-a-service model, they can make more informed decisions, based on a near-real-time overview of how and where technology is used in their facility. This enhanced data visibility can also help spark valuable discussions among staff members who are involved in clinical care – for example, in the form of structured kaizen events that can help to identify workflow improvements for everyone’s benefit. No longer do different stakeholders have to rely on gut feelings. Instead, they can ask: what is the data telling us?

The future of healthcare is as-a-service
Taken together, these benefits illustrate why the transition to as-a-service models in healthcare is expected to gain further traction. And this transition doesn’t need to be an abrupt one. Hybrid as-a-service models allow healthcare leaders to retain ownership of hardware while still benefiting from more flexible fee structures and enhanced partner services, with the ability to completely shift ownership over time. This hybrid ownership and fee structure enables healthcare leaders to continue asset depreciation preferences, while also investing in an as-a-service model for analytics, clinical improvement and technology management. As the organizational needs of healthcare leaders evolve over time, the model can evolve with them. Twenty years ago, no one could have foreseen the full impact that as-a-service, subscription-based offerings would have on the way we consume media, software, and other products today. Could the impact on healthcare be just as transformative?
References [3] https://healthsystemcio.com/progressive-thinking-patient-monitoring/ [5] Results from baseline and post time and motion studies conducted by Philips and Florida-based customer’s internal teams across critical, mid and low acuity care areas (or units). Other results from surveys conducted pre- and post-Philips installation of patient monitoring system at one Florida hospital. Results are specific to one facility, actual results for other health systems may vary.
Stay up to date and subscribe
Sign up to stay informed and receive information on healthcare innovation, straight to your inbox